How the Healthy Opportunities Pilots Created an Ecosystem of Care
Reema Health sat down with Amanda Van Vleet, Associate Director, Innovation, in the North Carolina Medicaid Strategy Office to discuss the Healthy Opportunities Pilots, which are the first initiative in the United States to allow a Medicaid program to fund a wide range of health-related services addressing nutrition, housing, transportation and interpersonal violence (IPV)/toxic stress—to a broad range of eligible populations including children, pregnant women and adults enrolled in managed care through a fee schedule.
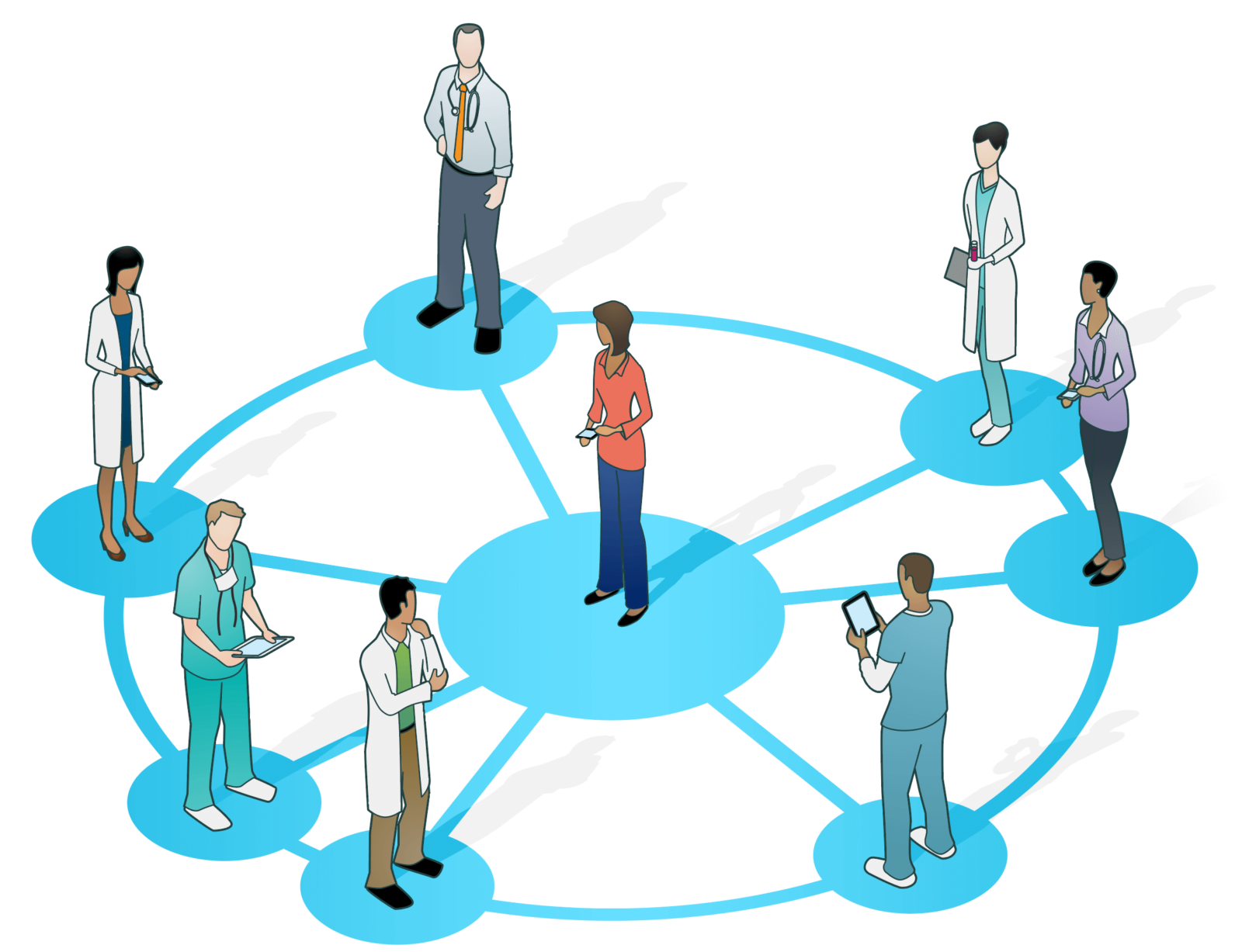
In our conversation, Amanda shared how her office created an ecosystem of care in collaboration with a wide range of entities to support programs that address Social Determinants of Health (SDoH) associated with health outcomes.
Tell us about North Carolina’s approach to developing the Healthy Opportunities Pilots.
Amanda:
A lot of the groundwork for the Healthy Opportunities Pilots was established over the last six years. Around 2017, we were directed by the state legislature to implement Medicaid-managed care, and around that time, Mandy Cohen was appointed as the new secretary of North Carolina’s Department of Health and Human Services. She has a healthcare financing background, and a personal interest in social drivers of health as well as addressing whole person health. She wanted to take the opportunity to create a Medicaid program for North Carolina through managed care, and her approach was to create the best managed care program in the country through a focus on whole person health, including behavioral and social health.
Her approach to creating the program was to create a core infrastructure and tools that all North Carolinians can use. We have a standardized list of SDoH screening questions and a statewide closed-loop referral platform. She also wanted to work into our Medicaid waiver requirements for health plans to use the infrastructure and tools we created for their Medicaid populations with the hope that the plans will also use those for their Medicare commercial populations and individual market populations.
Once that system was in place, then the missing piece was healthcare financing for social services. Our approach was to leverage federal dollars through Medicaid, and we asked for that as part of our 1115 waiver. By moving from fee-for-service to managed care, Centers for Medicare & Medicaid Services (CMS) allowed us to take a portion of those savings and use $650 million for the Healthy Opportunities Pilots.
What about North Carolina and its population makes it an important location for this type of program?
Amanda:
It has been important for us to show that a southern state can think creatively about how to address whole person health and to be a leader amongst our other state partners in the South. Our Healthy Opportunities Pilots is currently taking place in three regions within the state, and they are all predominantly rural, so this is also significant as a rural health initiative.
It has been important for us to show that a southern state can think creatively about how to address whole person health and to be a leader amongst our other state partners in the South.
Because the state has both urban and rural areas, North Carolina is representative of many other states, and can model how to address some of the challenges inherent in understanding populations with different needs and identifying how to meet those needs. In the next iteration of the Healthy Opportunities Pilots, we plan to expand services to more urban areas. My hope is that as we expand, the pilots will be something states with both urban and rural areas can emulate and replicate.
In terms of implementation, who are the key players in the Healthy Opportunities Pilots? What are their roles?
Amanda:
We developed what we call an ecosystem model, which is a regional model with different types of entities. Each entity has a distinct role to play within this community health effort. Right now, this includes three regions which encompass thirty-three counties of North Carolina’s 100 counties, which represents a third of the state. Within that, there are currently five health plans, but we plan to add four more in the near future. We have five clinically integrated networks, twenty-three care management entities, and three network lead organizations, which are community hubs that build networks of community based organizations and contract on their behalf with the health plans. There are currently 150 community based organizations participating in the pilots.
One of the most interesting things I’ve noticed as these partnerships develop is that every type of entity, including the state, is learning to operate differently in order to think about social services as a part of our Medicaid program.
One of the most interesting things I’ve noticed as these partnerships develop is that every type of entity, including the state, is learning to operate differently in order to think about social services as a part of our Medicaid program. For example, our Community-Based Organizations (CBOs) are learning how to function in a healthcare context. With the health plans, we’re working to implement policies and operations that will be inclusive of CBOs that facilitate their participation, and instead ask a little bit more of our health plans to offset the administrative lift that might be a struggle for a small organization.
That sounds like a significant reset of the dynamic between health plans and CBOs. How has that shift changed conversations, especially around the member experience?
Amanda:
All of our partners have been supportive of the concept that SDoH contributes to health. When we started talking about what that looks like on the ground and in practice, we realized how difficult this would be for all entities—health plans, providers, and community-based organizations—so the State did play a role in coordinating requirements across all of our partners. To do that successfully, we aimed to keep the member’s experience top of mind for all entities. We also aim to prioritize the needs of some of our least-resourced organizations. The Network Leads have been a really important partner for advocating on behalf of, and supporting, the CBOs.
What aspects of your approach could be adapted by other states?
Amanda:
I’m a big fan of our network lead model. While some states have taken a more direct approach to having CBOs contract with health plans, our network leads have been instrumental in providing technical assistance and training to CBOs and advocating for them to our health plans. New York is adopting that approach, and other states have recently asked us for information on it.
Payment to CBOs is something we’ve given a lot of thought to, since we’re asking CBOs to change how they are being compensated on a day-to-day basis. We prioritized making that process as simple for them as possible. For example, we have them invoice rather than use a standard claims software, and the State and our partners do the work of translating those invoices to claims. It was really helpful for the state to step in and take a role there in order to get the participation that we wanted.
At the core of our efforts, we’ve taken a learning mindset: it’s a new initiative, and we have to start somewhere. If we waited until everything was perfect, we would never launch, so we started where we could to get things off the ground and are continuously trying to make improvements to the program based on feedback.
We also sought out stakeholder feedback early and often. We conduct a lot of focus groups with CBOs, plans, and providers, and engage them regularly to learn more about which aspects of the pilots are going well, and which could be improved. At the core of our efforts, we’ve taken a learning mindset: it’s a new initiative, and we have to start somewhere. If we waited until everything was perfect, we would never launch, so we started where we could to get things off the ground. Since then, we’ve been working to continually improve capabilities as we go and to take a broad view of success. For example, our CMS evaluation is measuring improved health outcomes and lowering healthcare costs, but we’re also thinking about how we establish partnerships and infrastructure so that this work can continue after the pilots are completed.
Looking for more? Part two of our interview with Amanda focused on the “how” of financing SDoH activities and a closer look at the Health Opportunities Pilots is now available.



